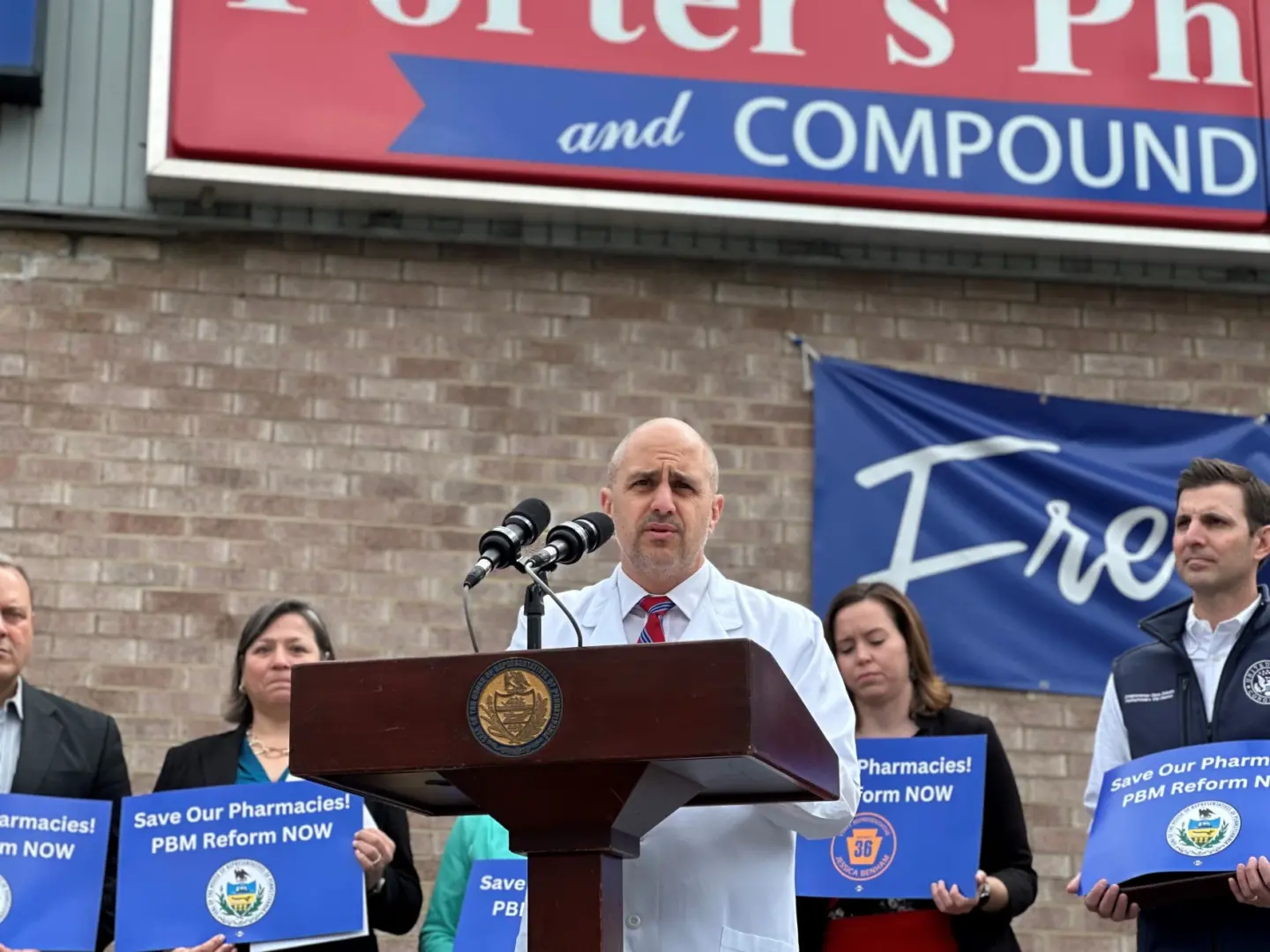
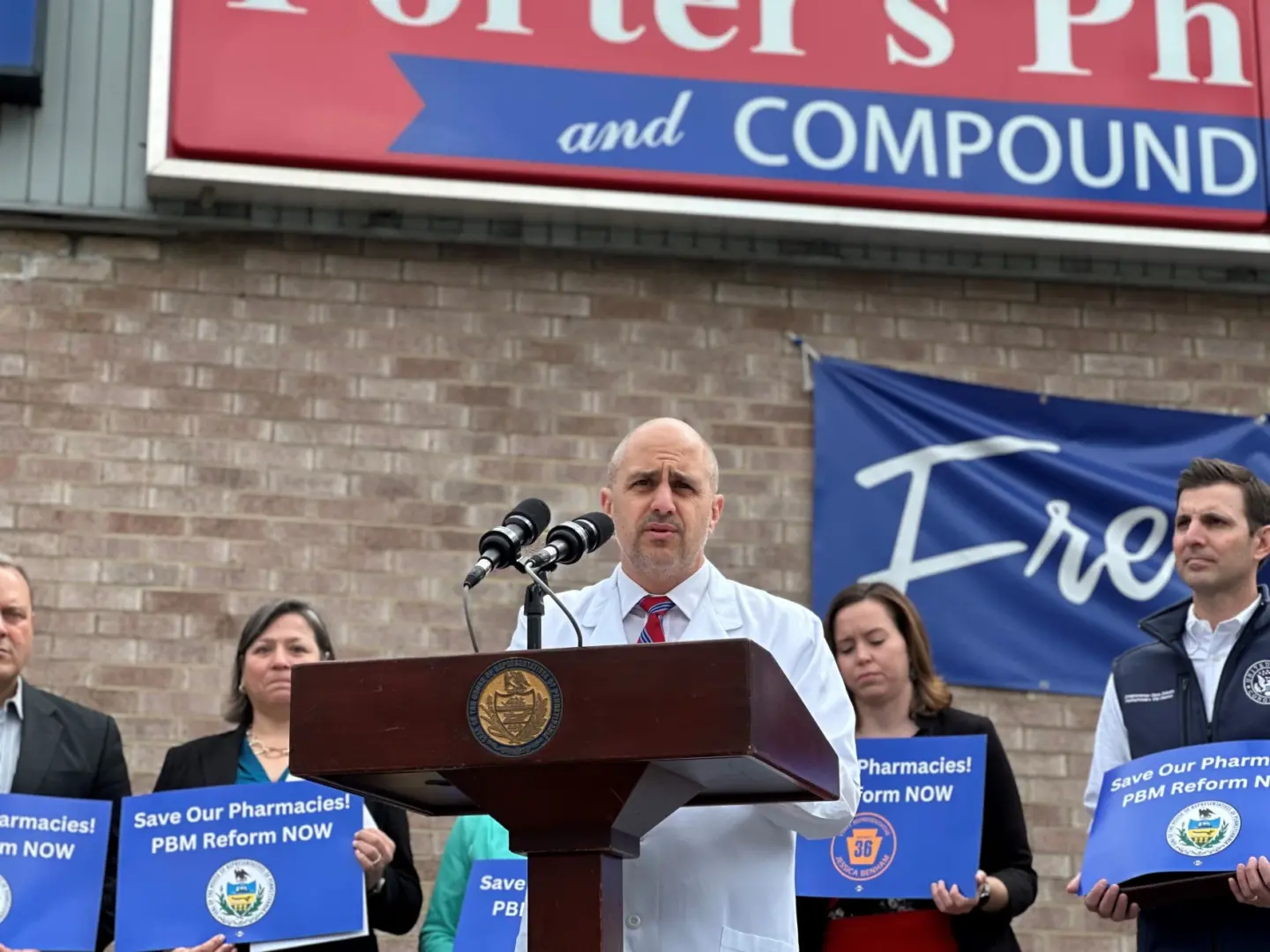
Eddie DeCaria, co-owner of Porter's Prescription Pharmacy, speaks during an April press conference about how his business has been impacted by pharmacy benefit managers.
Kiley Koscinski / 90.5 WESA
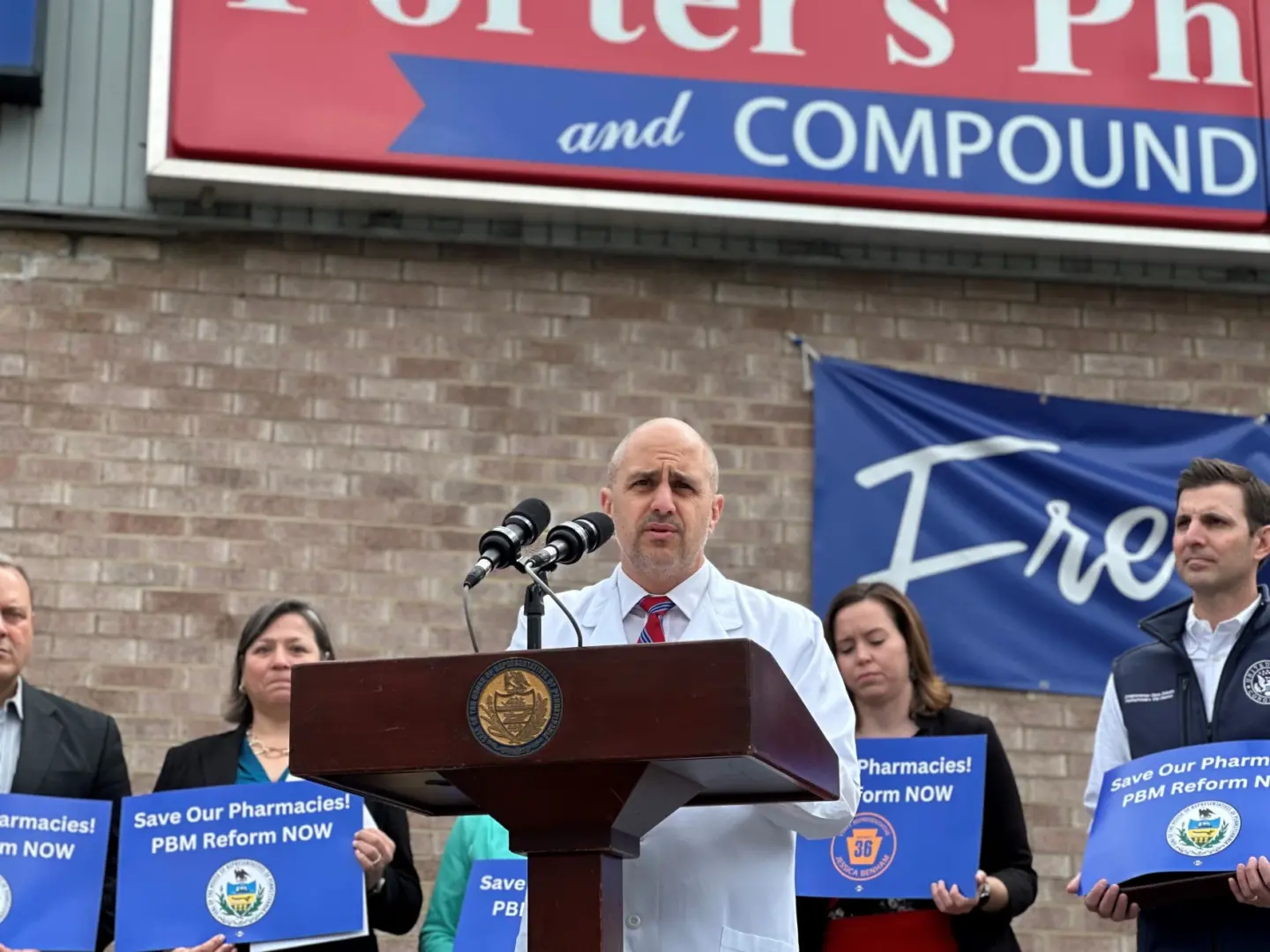
Eddie DeCaria, co-owner of Porter's Prescription Pharmacy, speaks during an April press conference about how his business has been impacted by pharmacy benefit managers.
Kiley Koscinski / 90.5 WESA
Kiley Koscinski / 90.5 WESA
Eddie DeCaria, co-owner of Porter's Prescription Pharmacy, speaks during an April press conference about how his business has been impacted by pharmacy benefit managers.
A bill that advocates say will help struggling local pharmacies compete with major chains is on its way to Gov. Josh Shapiro’s desk. The state legislature overwhelmingly passed a measure this week aimed at regulating pharmacy benefit managers (PBMs), which serve as middlemen between insurance companies and pharmacies and determine how much a pharmacy will get paid for the drugs it sells.
The bill was sponsored by Allegheny County-based state Reps. Jessica Benham (D-Pittsburgh) and Valerie Gaydos (R-Allegheny). Benham told WESA that getting the bill through the House and Senate is a “significant win.”
“What this all comes down to is leveling the playing field between big corporate pharmacies and the smaller ones in our communities,” she said.
PBMs were created to negotiate prescription drug pricing with drug companies through Medicaid to lower costs. They negotiate bulk discounts and fees with drug manufacturers, create lists of which medications are covered by insurance and reimburse pharmacies for prescriptions.
But community pharmacies argue they often receive reimbursement payments that don’t cover the cost of medications. And some blame PBMs for skyrocketing drug costs and a wave of neighborhood pharmacies closing up shop. Eddie DeCaria, co-owner of Porter’s Prescription Pharmacy in Moon, said he often loses money on certain prescriptions.
“A lot of pharmacies are living on borrowed time,” said DeCaria. “The state of industry now is in disrepair.”
He hailed passage of the bill and said he’s optimistic the state will continue to work on the issue.
“The war is not won and it’s going to take time,” he said. “This is round one.”
The legislation, HB 1993, enables tougher oversight of pharmacy benefit managers by limiting practices like patient steering, which channels prescriptions to a PBM’s own retail pharmacy. It also prevents them from requiring prescriptions to be ordered by mail, which often cuts out community pharmacies. The measure would also limit clawbacks by PBMs when a pharmacy makes a clerical error.
The measure did undergo changes in the Senate. Among the largest changes was a provision that delayed action on “spread pricing,” in which a PBM charges an insurer a higher rate than it pays the pharmacy and pockets the difference. Benham and Gaydos’ bill would have banned the practice. The Senate version instead calls for a broader study into the issue.
DeCaria lamented the change. He said often he could be reimbursed $900 for a drug that costs his pharmacy $1,000.
“People aren’t going to be able to [wait] for a study to show that we’re losing money right and left,” he said. “Look back this year alone. How many pharmacies have closed in Pennsylvania?”
(Benham said the answer is 140 community pharmacies statewide. The University of Pittsburgh’s ACT Pharmacy collaborative, which tracks closures across the country, has found similar trends nationwide. In an online statement it said pharmacies were “often the most accessible point of healthcare and the pace of closures “poses a grave public health risk.”)
Gaydos did not return calls for comment. But Benham said the Senate changes were a “compromise” and pledged to take more action in the future.
“These reports and studies are going to give us a sense of what other action we could be taking on the state level to protect our local pharmacies and save patients money,” she said.
The Senate version did add a new requirement that PBMs pay community pharmacies the same rate they pay their own affiliated retailers for prescriptions. It also requires that PBMs pass back 95% of any rebates they receive to the insurance provider.
State Sen. Judy Ward (R-Blair), who co-sponsored a PBM measure in the state Senate, said the bill was a meaningful step forward.
“Too many pharmacies are disappearing in Pennsylvania and the time is now for meaningful reform to the relationship between pharmacies and pharmacy benefit managers,” Ward said.
CVS Caremark, one of the three major PBM companies, declined to comment specifically on the new rules. But a spokesperson said lawmakers should focus on reining in prices set by pharmaceutical companies.
“Any measure concerning prescription drugs must be judged by whether it reduces drug prices for employers and consumers,” said Phil Blando, a spokesperson for CVS Caremark. “We welcome the opportunity to work with legislators addressing the root cause of high drug costs: Big Pharma’s high list prices.”
Still, large PBMs appear to have been thriving. In the last decade, the state’s Medicaid spending on pharmacy benefits has increased from $1.4 billion to $3.7 billion, according to the National Community Pharmacy Association. Three PBMs — CVS Caremark, Express Scripts and Optum Rx — control 80% of the marketplace.
“Drug prices didn’t skyrocket overnight,” Benham said in a statement Thursday. “It’s going to take measures beyond [this bill] to make medicine affordable again.
“But putting corporate middlemen like PBMs in check is essential in giving power back to independent pharmacies and the patients they serve every day.”

A collection of interviews, photos, and music videos, featuring local musicians who have stopped by the WITF performance studio to share a little discussion and sound. Produced by WITF’s Joe Ulrich.
The days of journalism’s one-way street of simply producing stories for the public have long been over. Now, it’s time to find better ways to interact with you and ensure we meet your high standards of what a credible media organization should be.