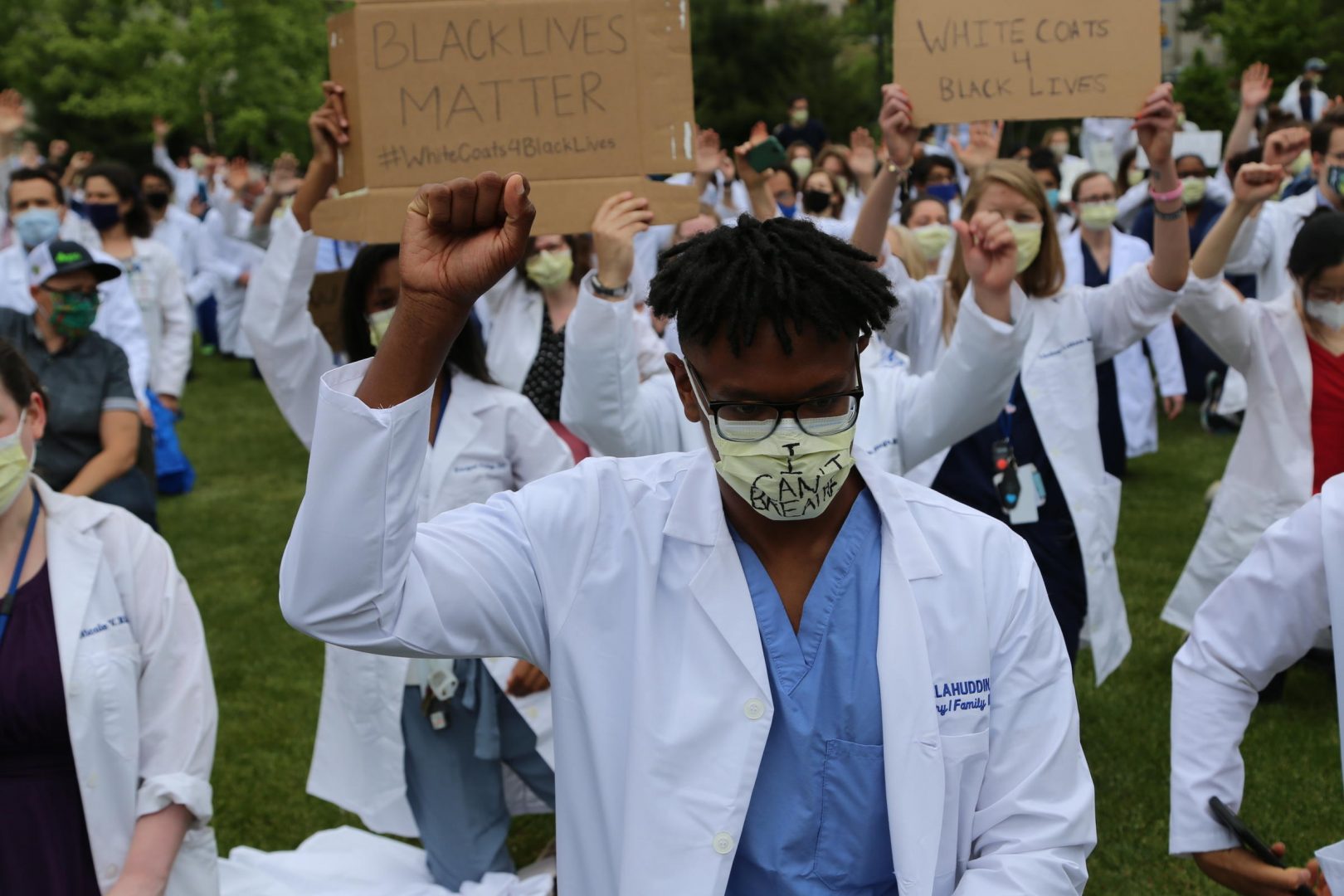
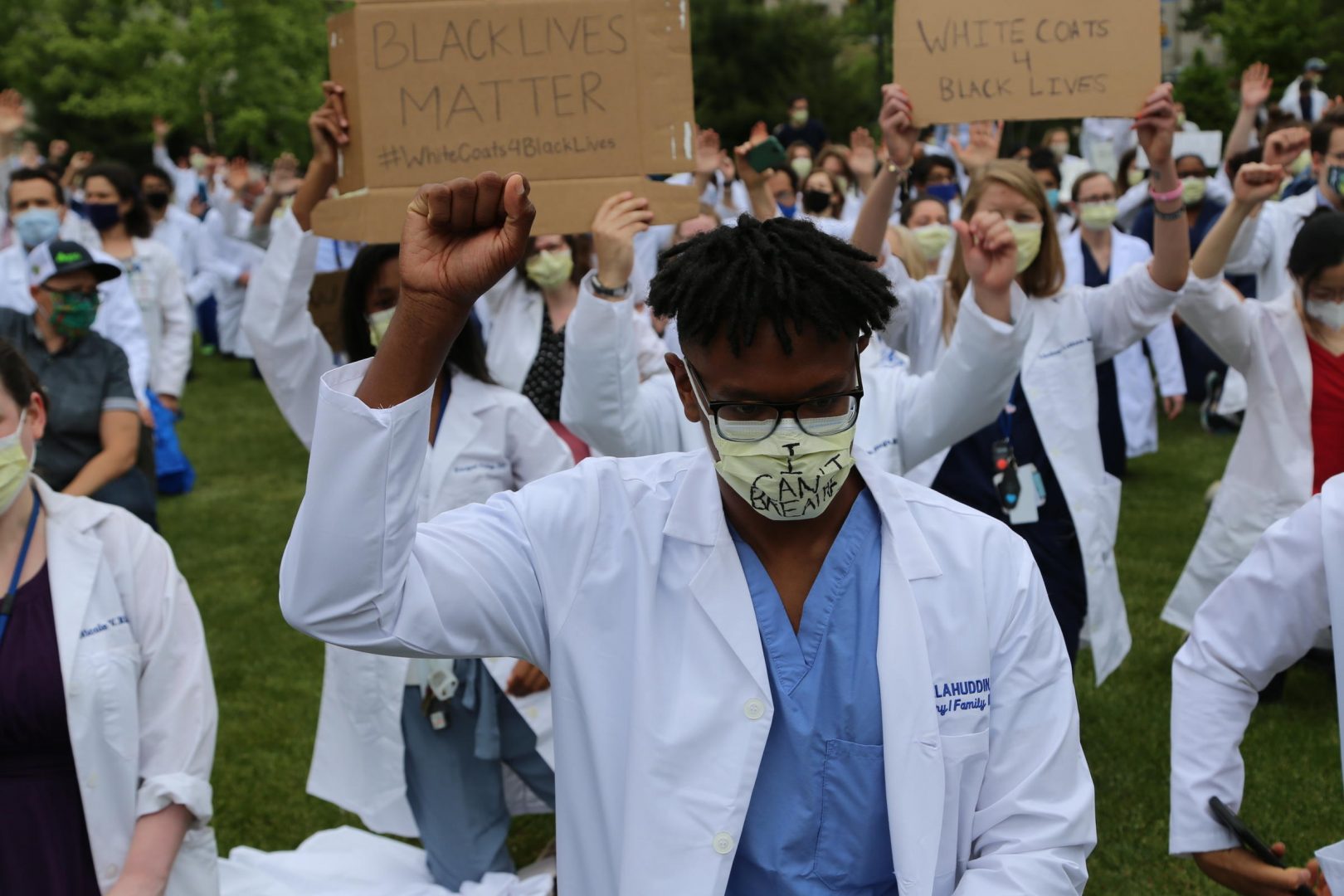
A health care worker raises his fist in solidarity with the Black Lives Matter movement during a demonstration in Oakland by White Coats for Black lives.
Katie Blackley / WESA
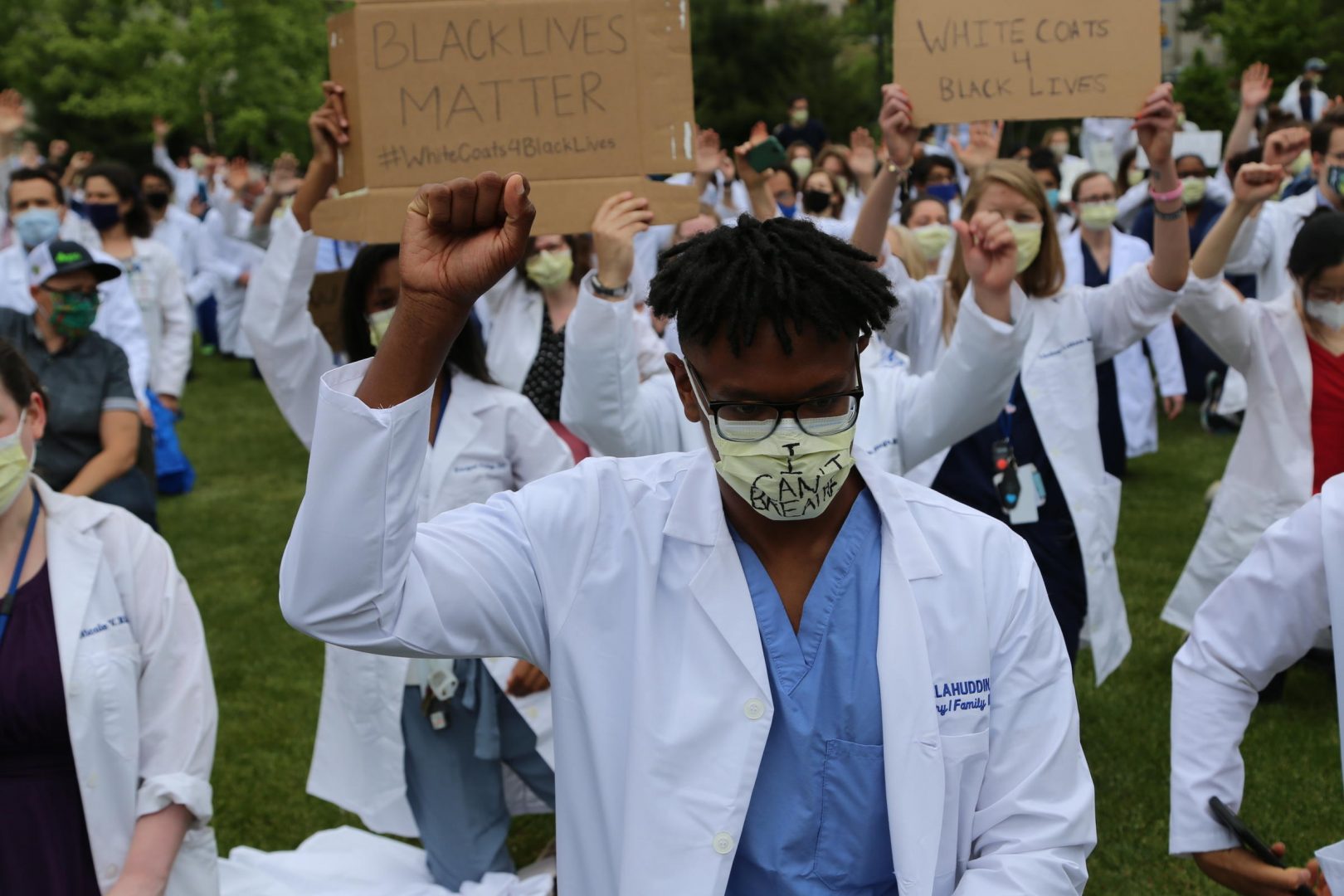
A health care worker raises his fist in solidarity with the Black Lives Matter movement during a demonstration in Oakland by White Coats for Black lives.
Katie Blackley / WESA
Katie Blackley / WESA
A health care worker raises his fist in solidarity with the Black Lives Matter movement during a demonstration in Oakland by White Coats for Black lives.
(Pittsburgh) — When public health historian Aishah Scott wrote her Ph.D. dissertation on the effects of the AIDS epidemic on Black Americans two years ago, she warned that even if a cure for HIV were found tomorrow, “A new disease would emerge wreaking the same havoc on the African American community.”
A year into the coronavirus pandemic, this virus has proven nearly twice as deadly for Black Americans than for white.
Scott is now a postdoctoral fellow in history at Carnegie Mellon University. She spoke with WESA health and science reporter Sarah Boden about the parallels between COVID-19 and HIV/AIDs. Scott said the fact Black Americans are more likely to experience housing insecurity puts this community at greater risk of contracting either virus.
This converstaion has been edited for length and clarity.
Sarah Boden: With COVID, it’s sort of straightforward, having a safe and stable place to live allows a person to isolate from others who might be infected with this respiratory virus. With HIV, the patterns of transmission are very different because the virus is spread through certain bodily fluids like blood or semen. So how does housing insecurity increase someone’s chances of contracting HIV?
Aishah Scott: Thank you so much for this question because it’s multilayered. One that people who have housing, one, will have more connections to care. Right? They are going to be able to go to a pharmacy and have a regular space to fill prescriptions. They’re more likely to have regular doctors that they can go to. So one, if someone does become infected they’re able to get connected to care. And we now know that people who are connected to care, and are able to get their [viral load] levels undetectable are not transmitting HIV when they have intercourse. So that’s one way.
Another way is that people who have housing instability are often in spaces in their relationships where they don’t, they’re not able to advocate for themselves in the same way. If someone’s in a domestically abusive situation, they don’t feel that they can necessarily tell their partner, “I’m not comfortable with the idea of having unprotected sex because I don’t know when was the last time you were tested,” or “I want you to get tested.” And also, the fear that if they’re not in a space where they can be autonomous on their own in terms of financial security, that they can’t, they don’t want to be put out on the street.
So, this shows the connection to how disability and in terms of employment security as well, having adequate, making a living wage and being able to support yourself and not be in a dependent situation in that way.
Katie Blackley/WESA
Boden: You mentioned employment and people who work outside the home are at higher risk for contracting the coronavirus. Many of these jobs are low wage positions. Are there similar patterns between employment and HIV?
Scott: Most definitely. The higher the poverty level, the higher the HIV infection rate. When we think about homelessness, or you think about housing insecurity, you’re thinking about people living in poverty and the most extreme forms of poverty. So, it makes sense that people who are lower income are having higher infection rates. People not having access to living wages and to jobs that provide them with adequate living arrangements, connections to health care, having jobs that don’t necessarily automatically qualify you for health care or great health care–you’re only able to do the bare minimum. Or it’s just not financially feasible. You’re making decisions as to whether or not you go to a doctor or you buy food. This puts people in a different dynamic.
Boden: I keep going back to the idea that the coronavirus and HIV, they’re just such different viruses. But the things that make people more, more vulnerable to these viruses are so similar.
Scott: This is how we see the hierarchy of socioeconomics that is impacting health outcomes. And that’s really the larger picture here, that we’re not just talking about these diseases, and I feel like that’s what happens. And that’s the misstep that happens every time there’s some sort of disease outbreak. Like this that we talk about the disease, but we don’t talk about the systemic issues that really make marginalized communities vulnerable. And we don’t talk about them with intention because it’s expensive to fix them.
Boden: Aishah Scott, thank you so much for talking with me today.
Scott: Thank you so much for having me. It was a pleasure to be here and to have these serious conversations about some very timely issues.
The days of journalism’s one-way street of simply producing stories for the public have long been over. Now, it’s time to find better ways to interact with you and ensure we meet your high standards of what a credible media organization should be.